The world’s population is getting older, with forecasts showing twice as many people aged over 60 years in 2050 compared to 2020. While living longer lives brings many benefits, it also requires adjustments to promote healthy ageing.
Older people with health issues such as obesity, diabetes, kidney problems or who are immunocompromised are at higher risk of serious illness and death if they develop flu or pneumonia. In contrast, those who are vaccinated are known to get indirect benefits, including reduced risk of heart attack, stroke and dementia.
Highlights at a glance
- Older people at at higher risk if infected by vaccine-preventable diseases
- The global population is ageing, posing challenges for health and social systems
- Vaccination policies, adult vaccine uptake, vary between European countries
- Europe need better monitoring of vaccination rates across all age groups
- FEAM calls for a harmonised adult vaccination schedule in Europe
The Federation of European Academies of Medicine (FEAM) is one of several scientific bodies advocating for vaccination in the context of healthy ageing and disease prevention. ‘A major challenge for immunising older adults is that people often mistakenly believe that vaccines are only for children,’ explains Dr Elisa Corritore, Director of Operations at the Federation of European Academies of Medicine (FEAM).
In a wide-ranging interview ahead of European Immunisation Week, Dr Corritore said the importance of promoting life-course vaccination is underpinned by the knowledge that ‘vaccines not only impact mortality, but also antibiotic usage, antimicrobial resistance, non-communicable diseases, and disability’.
To ensure higher awareness and uptake of vaccination among older people, and reduce differences between EU Member States, EU-wide efforts are needed to address practical barriers and vaccine hesitancy. Dr Corritore also calls for a unified vaccination schedule for older people.

Interview with Dr Elisa Corritore, Director of Operations at the Federation of European Academies of Medicine (FEAM)
From your research, what do we know about similarities and differences between adult vaccination policies across Europe?
In April 2021, FEAM launched a survey to its Academy network to obtain details of current vaccination schedules for older people in different European countries. The overall feedback clearly reflects the same data recently published by the European Centre for Disease Prevention and Control (ECDC): There is no harmonisation related to immunisation schedules between European countries.
Data on vaccination coverage is usually recorded in decentralised platforms or at regional level. The EudraVigilance register – operated by the European Medicines Agency (EMA) – provides data from across Europe, only on suspected adverse events. There is a need to harmonise vaccination programmes in adults over 65 years to favour healthy ageing and protect the old at-risk population. Such science-based vaccine initiatives could also reduce health care use of expenditure.

In our study, we stress the importance of having a unified recommendation for vaccination schedules for the old age in Europe. There are clear benefits to following this path, since it would increase trust in the population, bring clarity, facilitate the movement of individuals between countries and enable the supply chain to work better.
What are the factors driving vaccine hesitancy among older people? How is hesitancy in this group different from other population groups?
Vaccine’s acceptance varies across European countries. In Denmark, Portugal, and Spain more than 90% of the respondents considered vaccines to be safe. In contrast, in Latvia, Bulgaria, and Poland, more than 25% of the respondents had doubts about vaccine effectiveness.
The World Health Organization (WHO) developed a Tailoring Immunization Programs (TIPS) approach for the European Region in 2019. The approach helped to identify target groups (groups with low vaccine coverage), barriers and drivers to vaccination, and to design evidence-based interventions for high and equitable vaccination uptake. It is evident that there is a need to harmonise vaccination programmes in adults over 65 years to favour healthy ageing by bridging the existing adult vaccine gap and protecting the old at-risk population.
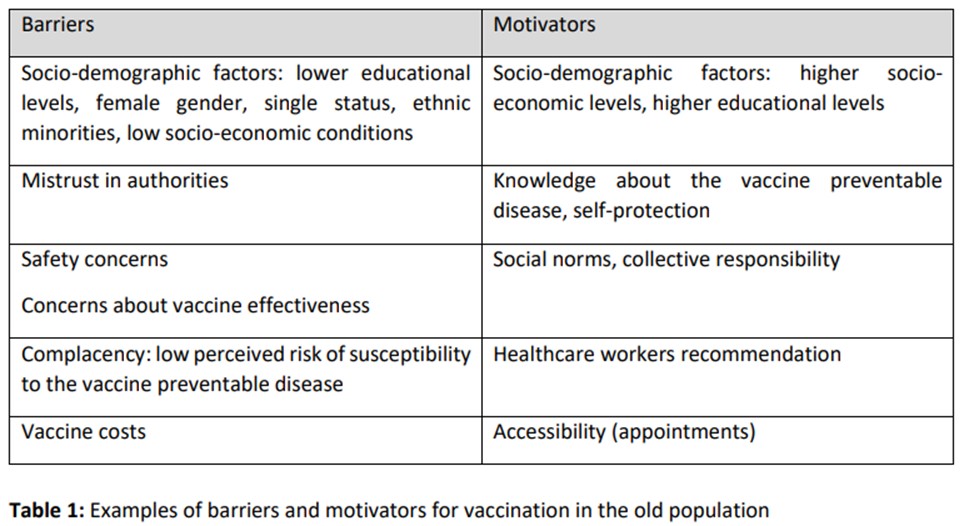
Key elements that could help improve vaccine acceptance would be increased education, trust, knowledge about vaccines and their safety, improved collective responsibility, policy on costs and improved management of infrastructure that facilitate accessibility to vaccination (see table below).
What can be done to increase vaccine uptake among older adults? Are there any good examples from European countries of how to get this right in terms of policy or communication?
Improving communication, implementing health education. A greater education may contribute to higher acceptance. Due to a lack of appropriate vaccine education, healthcare professionals also lack confidence in the efficacy of vaccines, do not fully appreciate the positive effects, and have doubts about the low risk of adverse side effects. Individuals at risk are often not encouraged by physicians regarding the specific and indirect benefits of vaccination. The success of future vaccine educational campaigns needs to target all healthcare professionals’ attitudes and perceptions in all types of workplaces.
In Europe, very few countries, except for the United Kingdom and the Netherlands, satisfy WHO recommendations (75% of the 65+ population) for annual influenza vaccination. Whereas countries such as Austria, Belgium, Germany, Greece, Italy, show the most complete vaccination programmes.
Why is it important to track adults’ immunisation status in Europe, as they do elsewhere? Who (which agency or authority) should collect and publish this data?
Monitoring is crucial for public health issues and for the individual’s own health. The implementation of a European electronic data system – similar to the Adult Immunization Status (AIS) in the US – would be a big step and this was already suggested.
A system that tracks the percentage of members 19 years of age and older who are up to date on recommended routine vaccines for influenza, tetanus and diphtheria (Td) or tetanus, diphtheria and acellular pertussis (Tdap), zoster and pneumococcal. Vaccination records provide a history of all the vaccines you received as a child and adult. This record may be required for certain jobs, travel abroad, or school registration but also it would be helpful to predict and calculate coverage rate across Europe.

The European Council Conclusions in December 2022 (Czech Presidency) put the spotlight on adult vaccination. What was your response to this and what must be done now to deliver on these goals? What can FEAM/academies do to support this?
FEAM has welcomed this important vision which highlights the urgent need to fight vaccination hesitancy, while strengthening EU cooperation for the future.
Each Member State develops its own life-course vaccine recommendations, and this leads to differences on vaccine age thresholds, programmes, and national reimbursement. FEAM strongly advocates that in the current COVID-19 era, the time is right to increase vaccine diplomacy to reaffirm a collective commitment to European adult immunisation based on population growth, infection frequency and scientific advances in vaccinology.
FEAM will continue to provide the best scientific evidence on how this could be implemented, with the support of our academies. The academies have an important role to play in bringing this evidence to national policy makers and legislators, but also in sharing good practices.
Read more: Immunisation for old adults in Europe: scientific and social strategies



