 “The good news is we are living longer,” says Dr Daphne Holt, Vice President of the Confederation of Meningitis Organisations (CoMO). “The bad news is we’ll have to work longer which is all the more reason to stay healthy.”
“The good news is we are living longer,” says Dr Daphne Holt, Vice President of the Confederation of Meningitis Organisations (CoMO). “The bad news is we’ll have to work longer which is all the more reason to stay healthy.”
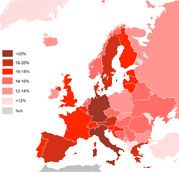
Speaking at a pre-conference session of the European Public Health Conference in Glasgow, Dr Holt said the greatest increase in Europe’s population in the coming decades will be in the oldest age groups.
“The average life expectancy for babies born in 1960 was about 69. Now it’s gone up 10 years thanks to better healthcare, better workplace safety and better nutrition. The strongest growth will be in the 85+ age group,” she said.
The implications of having growing numbers of older people and a shrinking middle-aged population are potentially stark.
“Age-related spending is projected to rise to 29.1% of GDP by 2060 and the greatest increase of all age-related spending over the next 50 years will be on healthcare,” Dr Holt told the meeting. “A healthy older population will reduce healthcare costs and help to alleviate pressures on national health systems.”
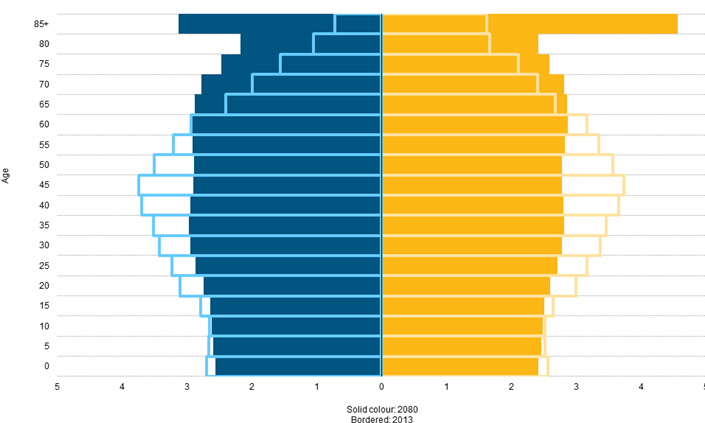
Figure 1: Population pyramids, EU-28, 2013 and 2080 (% of the total population) – Source: Eurostat
But Dr Holt had another dose of good news. “By staying healthy as we get older, we’ll have more time to enjoy ourselves,” she said. “My worst nightmare is to retire and die. This is my play time.”
Box 1: SAATI Report
A report by SAATI – Supporting Active Ageing Through Immunisation – has highlighted the value of adult immunisation in an ageing population.
Key recommendations
- Incorporate life-course immunisation into healthy and active ageing policies, public health and prevention strategies.
- Expand opportunities for citizens to receive vaccination
- Improve the leadership of health professionals
- Strengthen health literacy and public communications
- Enhancing surveillance and monitoring
The SAATI Partnership comprises patients’ and professionals’ associations, clinicians and ageing specialists.
Adopting a healthy lifestyle significantly improves our chances of ageing well. “We’re told we need to eat better and exercise more but the easiest step is to be vaccinated against preventable diseases,” said Dr Holt.
While vaccination is often associated with routine childhood immunisation, adults can have vaccines against a range of diseases such as influenza, pneumococcal disease, tetanus-diphtheria-pertussis, chickenpox and shingles, meningococcal disease, measles-mumps-rubella and human papillomavirus.
The WHO estimates that between 600,000 and 800,000 adults die every year from pneumococcal disease; more than 90% of flu deaths in the US are in persons aged 65 and over; and almost half of US measles deaths are in adults.
So why is adult immunisation still under the radar?
Dr Holt said healthy adults are much less likely to have contact with health services and tend not to think about vaccine-preventable diseases unless they are directly affected. For similar reasons, many preventable diseases do not have ‘champions’ to help raise public awareness.
“That’s why we launched a platform of patient groups, health professionals and policymakers – Supporting Active Ageing Through Immunisation (SAATI),” she said. The SAATI Partnership published a report at the European Parliament in November 2013 highlighting the burden of infectious diseases in adults (see box 1).
Spotlight on pneumococcal disease
The incidence of invasive pneumococcal disease – and associated hospitalisation rates are significantly higher in the over 65s, representing a rising burden as the population ages.
Professor Hartmut Lode, Research Centre Medical Studies, Berlin, Germany, said community-acquired pneumonia (CAP) is a particular concern for older people.
The risk of hospitalisation due to CAP increases steadily with age. The biggest burden is seen in the over 85s – precisely the age group where Europe’s population is set to see strongest growth.
“Mortality from pneumonia, including CAP, increases dramatically aground the age of 55,” Professor Lode says.
However, while the very young and the very old have the highest death rates from invasive pneumococcal disease, most children are vaccinated against pneumococcal disease as part of the standard immunisation schedule. Older people are often overlooked.
The risks are higher still for older people with chronic conditions such as cancer, lung disease, diabetes and heart problems. “We call this the toxic mix – the ageing patient who is suffering diseases like COPD, diabetes, ischaemic heart diseases, smokers and is then picks up a pneumococcal infection,” says Professor Lode.
He said improved surveillance can help to reduce the impact of CAP but avoiding infection would be even more effective: “Prevention of infections is better than treatment.”
As well as the toll pneumonia can take on people and the healthcare system, it is a significant burden on the economy. Professor Lode said that pneumonia alone costs Europe more than €10.1 billion per year, while pneumonia and influenza combined are responsible for one third of the use of respiratory units in the EU.
Frustratingly, rates of adult immunisation against pneumococcal infections are low. Just one in ten adults over the age of 50 years has been vaccinated. Contrast this with the 49% of adults who are vaccinated against influenza and the 70% that have been vaccinated against tetanus and diphtheria.
| Economic burden of pneumonia in Europe | Cost per annum |
| Overall financial burden | € 10.1 billion |
| Outpatient care | € 0.5 billion |
| Drugs | € 0.2 billion |
| Indirect costs from lost work days | € 3.6 billion |
Professor Lode said adult vaccination is often low on doctors’ ‘to do’ list and can be a blind spot for policymakers. A study exploring the reasons why physicians do not prescribe pneumococcal vaccines in line with European and national guidelines shows that most only target high-risk groups. Others cite lack of time and competing priorities.
The research finds that public awareness of invasive pneumococcal disease is low. That’s why primary care physicians need to highlight the importance of vaccination when treating patients at risk of pneumococcal infections.
Prof Lode concluded that pneumococcal vaccination rates for adults are “far below desired targets” despite the significant impact the disease can have on patients and the wider economy.
More facts and figures and stats.
“Policymakers need to accept that prevention is not a cost but an investment. Sometimes the benefits of immunisation accrue over the long-term but with flu and pneumococcal disease the benefits are seen very quickly. The cost of vaccines is small so it is really a question of political will.”
European solutions to a European problem
Europe’s demographic trends pose a particular challenge that requires a shared solution. Yet the European Union has not been particularly proactive on health policy in the past. This, at least in part, is because the Treaty underpinning EU law reserves health policy as a matter for national governments – Brussels can make recommendations but ministers in London, Berlin and Paris and elsewhere call the shots.
However, there are signs that this could be gently shifting as experts and policymakers begin to recognise the value of working together on public health. After all, viruses have no respect for national borders so greater coordination between EU governments can benefit everyone.
Prof Lode called for more power to be given to the European Centre for Disease Prevention and Control (ECDC). The Stockholm-based EU agency is tasked with identifying, assessing and communicating current and emerging threats posed by infectious diseases.
He said the ECDC’s counterpart in the US – the CDC – has a more visible public presence. The CDC has the power to centrally coordinate vaccine programmes, develop and share scientific knowhow, and run large campaigns to boost public awareness.
Dr Holt agreed that more should be done at European level to drive change. This, she said, would require collaboration between policymakers, patient organisations and health professionals to communicate clearly about life-course vaccination.
Perhaps those words were ringing in the ears of national health ministers when they gathered in Brussels on December 1, 2014. The 28 ministers agreed new European Council ‘Conclusions’ on vaccinations, guided by the Italian government which held the rotating six-month EU Presidency in the second half of 2014.
The text, signed off by all European governments, makes several mentions of the need to take account of input from the ECDC and WHO. Ministers also agreed to encourage research aimed at “demonstrating the benefits of a life-course approach”.
Perhaps most significantly for those attending the European Public Health Conference in Glasgow, EU health ministers called on national governments to “consider immunisation beyond infancy and early childhood by creating vaccination programmes with life-long approach”. Demography demands that these words lead to action.
This report is based on a pre-conference session at the European Public Health Conference in Glasgow on November 19th 2014 organised bythe European Public Health Association. The event was facilitated and funded by Pfizer.




