Regulators, governments, companies and academics joined forces to develop Ebola vaccines. Now they have an even bigger target – SARS-CoV-2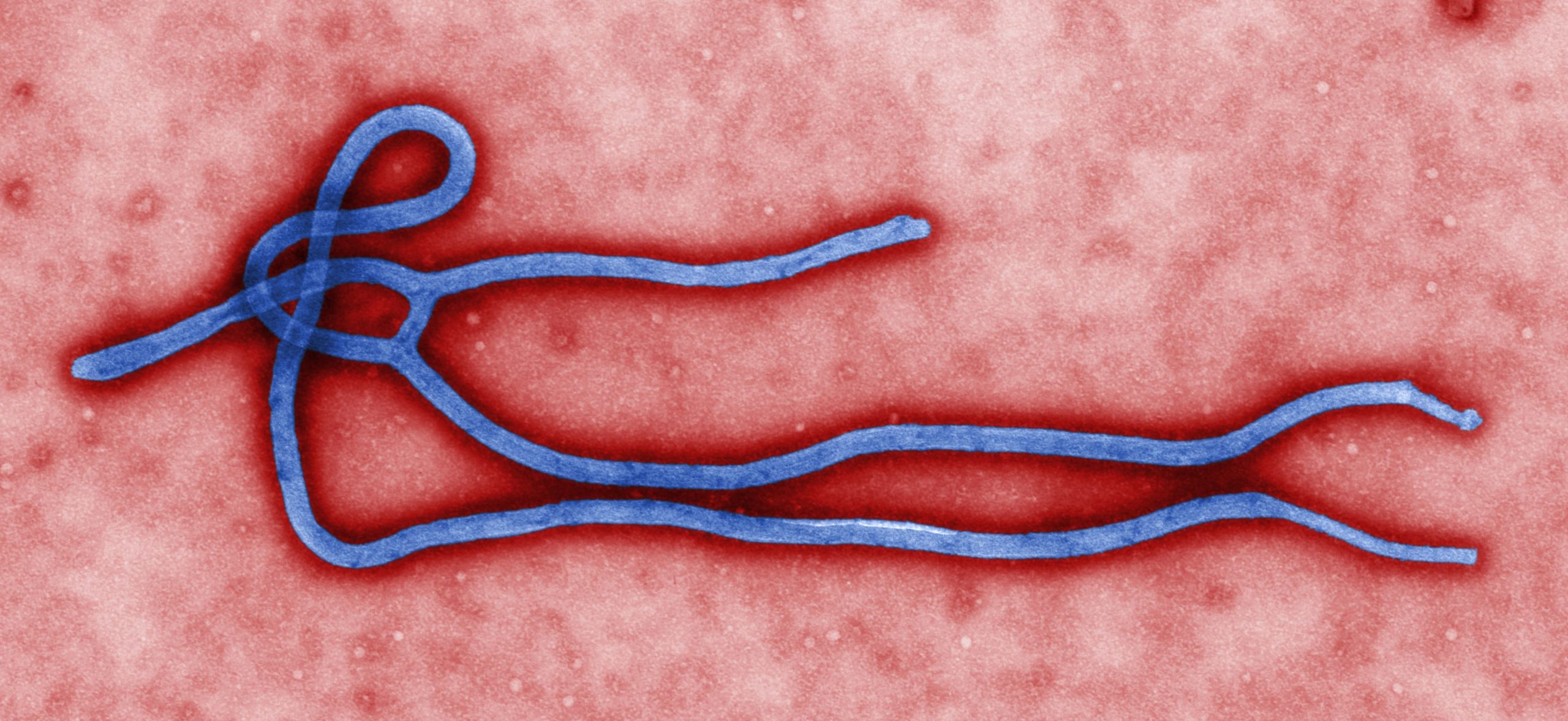
- Unprecedented partnerships tapped into expertise and funding to fight Ebola
- Innovative clinical trials accelerated development without compromising safety
- Two vaccines are now approved, helping to end the 10th Ebola outbreak in DRC
- WHO experts are exploring how vaccines could prevent resurgence rather than fire fighting epidemics when they strike
- Ebola experience holds lessons for developing vaccines against COVID-19
In 1976, a new virus was discovered in what is now called the Democratic Republic of Congo (DRC). The disease, which killed a large number of those infected, was named after the nearby Ebola river.
In the years that followed, the virus has caused tens of thousands of deaths in more than 30 outbreaks. Since the 1990s, the outbreaks have become more frequent and affected growing numbers of people, almost exclusively in Africa..
The worst epidemic to date was in West Africa from 2014-2016, during which more than 11,000 people died. The second worst outbreak began in 2018 in the DRC where 2,000 of the 3,000 people affected have died.
However, after decades of grim news, the world has recently recorded some hard-won successes against Ebola. It may even hold lessons for how to defeat other infectious diseases, by illustrating the scale of global cooperation required to rapidly develop and deploy new vaccines.
Ebola: a unique challenge
Ebola and SARS-CoV-2 (which causes COVID-19) are very different viruses. SARS-CoV-2 causes mild illness in most people infected and can spread quickly through droplets and through the air.
Ebola spreads through infected blood or bodily fluids. The average case fatality rate is around 50%, but ranges from 25% to 90%. Because it kills so many of those infected, its ability to infect new people is limited – many victims become ill soon after infection and die from their symptoms. In contrast, SARS-CoV-2 can be carried and spread by asymptomatic individuals.
However, some of the core principles of containing an infectious disease can be applied to both viruses: handwashing, contact tracing and isolating infected individuals. There are other parallels – many of those affected are healthcare workers who were exposed through close contact with sick patients. They are among the first in line for Ebola vaccines and will have priority access to future vaccines against COVID-19.
Vaccine research
Research on Ebola vaccines can be traced back decades. However, just as with coronaviruses, interest in Ebola research rose and fell in line with outbreaks. The Ebola epidemics of the 21st century had a major impact on affected areas and helped mobilise global scientific efforts to find a vaccine.
The first vaccine against Ebola was approved by US and EU regulators in 2019 while a second vaccine was given the green light in Europe in 2020. Both had already been deployed on the front line and have helped to contain outbreaks.
Along with academic and industry researchers, their development owes a lot to regulators. The European Medicines Agency says it has been providing technical advice to Ebola researchers since 2014. The EU medicines watchdog worked with the WHO to evaluate vaccines and ensure trials were designed to collect a large amount of data quickly without compromising on safety.
By vaccinating close-contacts of infected patients, along with healthcare workers, the spread of the virus was stopped. This so-called ‘ring vaccination’ has proven an effective way of curbing an outbreak.
However, new outbreaks continue to occur. While the DRC’s 10th Ebola outbreak is over, the 11th outbreak was declared in June 2020 and continues in another province. These are separate outbreaks, caused by genetically different viruses, according to the WHO. according to the WHO.
The response of international agencies and humanitarian organisations continues. Meanwhile, WHO experts are considering new strategies to make better use of the two approved vaccines and are expected to update their recommendations later this year. The current approach of pop-up vaccination (against sudden outbreaks) and geographic vaccination (in areas close to those enduring an epidemic) could be complemented with a more preventative strategy.
This would involve vaccinating people in at-risk countries before cases are reported. However, that would require millions of doses of vaccines and heavy investment in infrastructure (including fridges) and involve training large numbers of healthcare workers to deliver the vaccines.
Value of vaccines
Despite the cost of developing and deploying vaccines, an effective Ebola prevention strategy would deliver enormous value to affected areas. Of course, it would save lives by preventing the spread of Ebola, but it would also have other benefits.
By removing the fear of Ebola, it would ease the pressure on health services and improve people’s chances of living normal, productive lives. This would spare healthcare professionals from death and ill-health, and allow clinics to deliver care more safely – including routine immunisation services.
Similarly, if vaccines can reduce the spread and risk of COVID-19, it will save lives but also allow a return to social and economic activity. That would be priceless.
Ebola shows not only how to respond to an outbreak but how the global community can collaborate on vaccine development – and the importance of working with local communities to ensure new vaccines are embraced where they are needed.