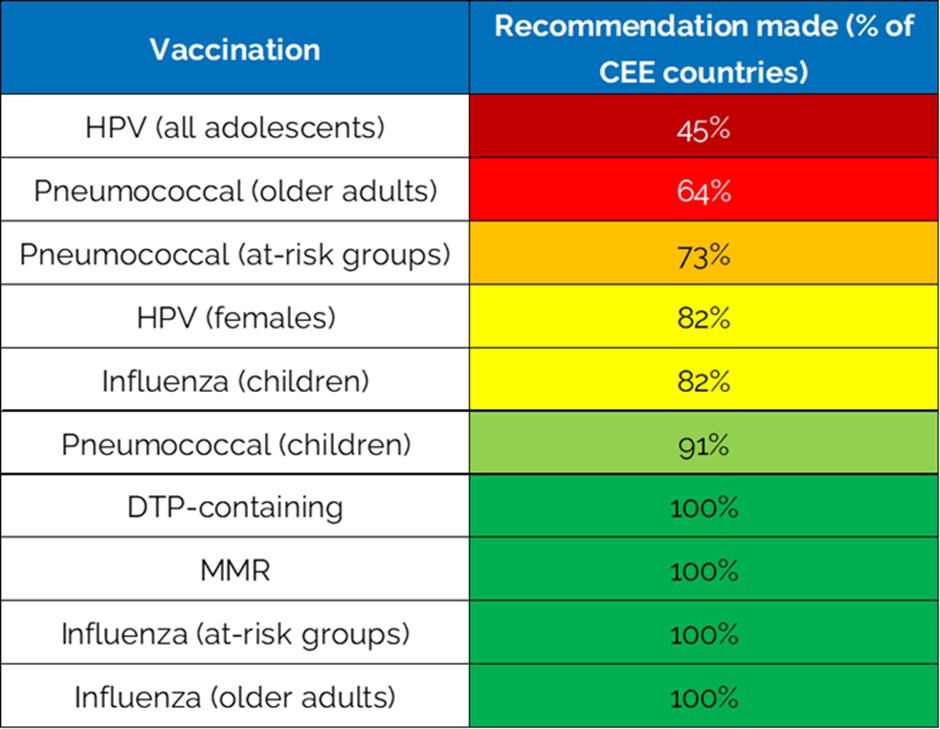
Vaccination rates in Central and Eastern European countries are lower than in some western European countries, particularly for vaccines that protect adolescents and adults. Low vaccine uptake can arise for a number of reasons, including affordability, access to vaccination and low levels of vaccine acceptance. EU data shows lower rates of vaccine confidence in Central & Eastern European countries.
A new report by the International Longevity Centre UK (ILC-UK) points to lower trust in health systems, low spending on preventative health, and a lack of recommendations for some vaccines.
ILC-UK, a founding member of the ILC Europe Network and the UK’s leading authority on longevity and demographic change, has published a new report ‘Shifting the Narrative: Improving vaccine uptake in Central & Eastern Europe’. The report asks: why are Central and Eastern European countries lagging behind the EU average; and how can we repair trust in governments and health systems to boost immunisation rates across Europe?
While only 21% of EU citizens report low levels of trust in their country’s healthcare system, this figure is 49% across parts of Eastern Europe.
Across the 11 Central and Eastern European countries studied in ILC’s new report (Bulgaria, Croatia, Czechia, Estonia, Hungary, Latvia, Lithuania, Poland, Romania, Slovakia, and Slovenia), healthcare spending has historically fallen behind that of other European nations.
In 2020, the average health spend per EU inhabitant was €2,110; in Romania, which had the lowest spend in this region of Central and Eastern Europe, it was €713.
It is easy to see how vaccination might be deprioritised amongst the wealth of other demands on health budgets if uptake lags. Health interventions are not taken without effective awareness campaigns and health system infrastructure to deliver them.
The report determined that the following factors together explain why vaccine uptake lags in the Central and Eastern Europe compared with the rest of the EU:
Low trust: lack of engagement from politicians, and a disjointed response to COVID-19 in several countries, has led to a breakdown in trust and reduced public confidence in vaccination.
Historical determinants: distrust in authorities often stems from previous forms of government and politics that restricted individual freedoms.
Poor communication: vaccination communication is often too little too late and has been subject to anti-vaccination rhetoric which too often goes unchecked.
Inaccessible health services: inadequate access and poor funding for vaccination is indicative to some that vaccination is not a priority for the government, and therefore individuals need not prioritise it.
Lack of health education: low awareness and lack of engagement on vaccination means many citizens in this region don’t prioritise it.
The interventions needed to address this disparity in vaccine uptake are varied and relevant to all aspects of healthcare. The report makes recommendations for action at the national and EU levels, and advocates for a whole-society approach to increasing uptake.
Health leaders, clinicians, religious and community leaders, pharmacists, and many other stakeholders have a part to play in normalising vaccination and helping others to understand its importance.
Key recommendations
- Invest in systems designed for prevention: patients, healthcare workers, and policy makers require seamless access to appropriate information to support improved access to, and uptake of, vaccinations.
- Take actions to inspire and engage: the benefits of immunisation should be clearly communicated and communication should be consistent at all levels of society.
- Democratise access to prevention: infrastructure at each level of the healthcare system should promote preventative interventions; this is part of the overall effort to ensure that health outcomes do not vary by wealth.
- Support the effective use of technology: digital communication tools should be used to reach underserved groups and counter anti-vaccine narratives that are too accessible online.
To read the report and its recommendations in full, click here
For more on ILC’s work adult immunisation, click here




