The number of women dying of cervical cancer would be close to zero within a generation under Europe-wide efforts to tackle preventative cancers. The plan includes concrete targets to ensure 90% of girls have the HPV vaccine, which prevents most cervical cancers, and to increase screening, testing and treatment.
However, progress varies widely across Europe. Some countries, including those with the highest rates of cervical cancer, have low vaccine uptake. Now a broad coalition of campaigners are coming together to turn the tide.
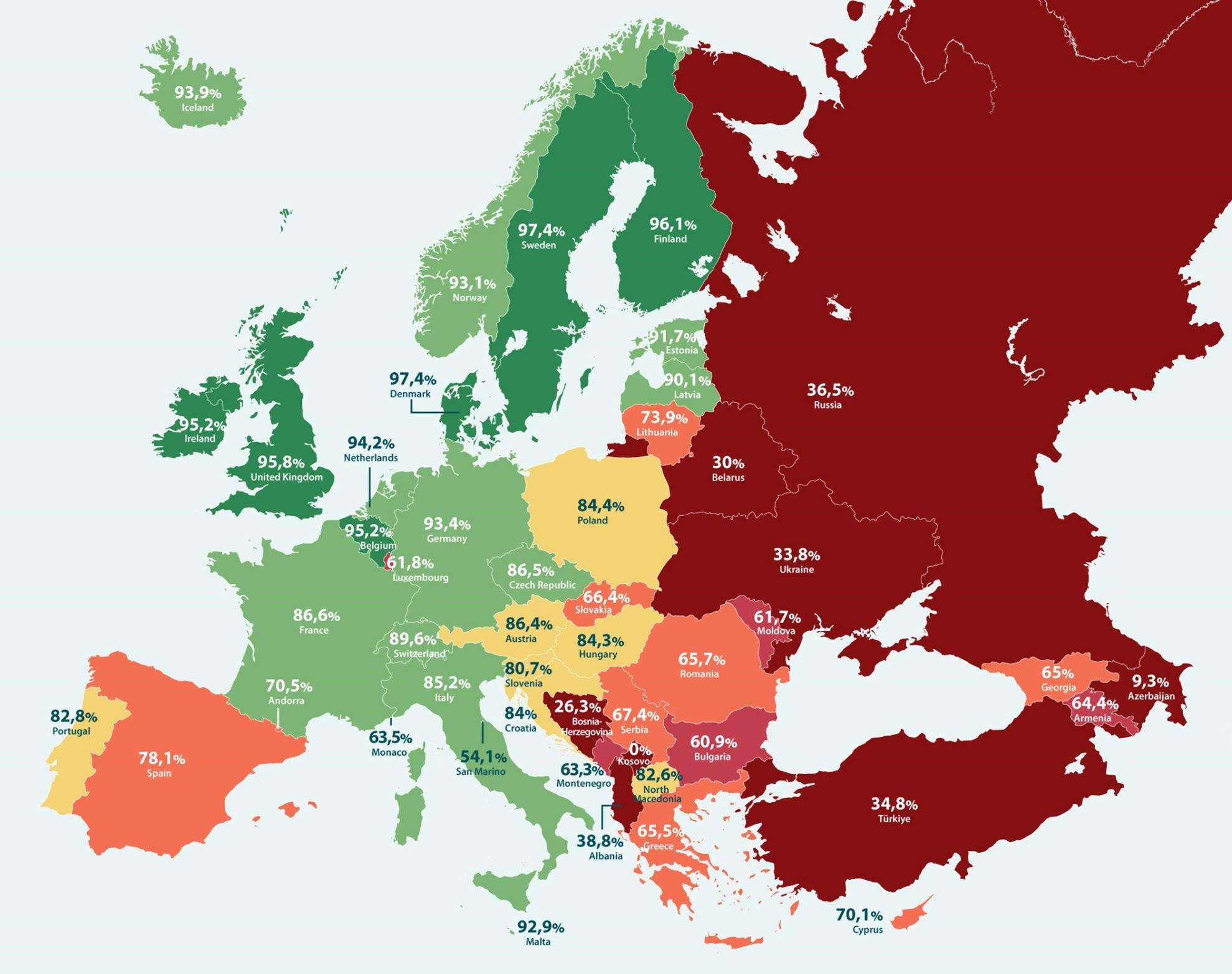
The scale of the challenge is illustrated by the HPV Prevention Policy Policy Atlas which grades national policies on HPV elimination. There is a clear geographic divide between the best performing countries (Denmark, Sweden, Finland, the UK, and Ireland) and those at the bottom of the table (Kosovo, Azerbaijan and Bosnia-Herzegovina).
The performance of several EU countries is also worrying, notably Bulgaria, Romania and Greece. However, these countries can take heart from the fact that some of the countries that now have high levels of HPV vaccine uptake have faced challenges in the past, including Denmark and Ireland.
The Atlas was developed by the European Cancer Organisation (ECO) and the European Parliamentary Forum for Sexual and Reproductive Rights (EPF). Neil Datta, Executive Director of EPF, said sharing information contained in the Atlas would shine a line on the situation across the continent.
‘This data demonstrates the wide range of HPV prevention policies in place and where significant improvement is needed,’ he said. ‘We hope it gives policymakers and politicians the information they need to implement changes, including for gender-neutral vaccination and cervical cancer screening across Europe.’

While vaccinating girls remains a priority, the value of increasing vaccination among boys ‒ particularly when uptake in girls is below target ‒ is significant as it contributes to lower circulation of the virus in the community. This can reduce girls’ exposure to HPV-related cervical cancers, but also helps to protect boys against head & neck and other cancers caused by the virus.
Most European countries are currently offering two doses of the vaccine to girls and boys (check your country’s schedule here). However, the WHO says a one-dose or two-dose approach can offer ‘durable protection’. This provides policymakers with more options when considering how to extend the impact of their immunisation programmes.
Sharing success stories
For its part, ECO’s HPV Action Network has just launched a new Protect-Europe hub to collect and share research and good practices from across the EU. It has also hosted events in the Parliaments of Croatia, Romania and Bulgaria, to encourage greater attention from policymakers.
ECO Chief Executive Mike Morrissey said targeting vaccine-preventable cancers is a ‘no brainer’ and he highlighted the efforts of politicians, youth organisations, oncology associations, sporting groups and patients to keep the issue on the political agenda.
National policy responses
At a webinar organised by ECO, experts from three countries outlined the state of play in their countries and ongoing efforts to improve prevention.
- Romania has the highest cervical cancer incidence and mortality rate in Europe, but low levels of vaccination and screening. Dr Carmen Ungurean, National Institute of Public Health, Romania, said survey data points to low awareness of HPV and vaccination in Romania. Following recent policy changes, HPV vaccines are now free for girls and boys aged 11-18, and 50% reimbursed for women aged older than 19.
- Dr Marija Posavec, President of the Croatia Society for School and University Medicine, said her country had faced significant difficulties sustaining high vaccine uptake. From 2007-2015, the HPV vaccine was recommended for girls but it was not free for most families. This set HPV vaccines apart from other recommended vaccines which are freely available. Anti-vaccine campaigners exploited this discrepancy and discouraged vaccination. From 2016, HPV vaccination was recommended for girls and boys aged 14-15 years. Uptake in 2023 was 51% in girls and 35% in boys.
- Prof Michail Okoliyski, Deputy Minister of Health, Bulgaria, said the anti-vaccine movement had targeted the HPV vaccine in his country, driving coverage down from 22% in 2013 to single digits by 2015 (5%). Last year it was just 1.5%, but current data suggest some improvement. Bulgaria aims to expand the target group to include boys and is working with GPs, gynaecologists, midwives and others to expand the impact of the programme.




