Flu season started early in the southern hemisphere this year and was particularly deadly in some countries. More than 430 people died in Australia while thousands required medical treatment in New Zealand.
The early arrival of flu season caught some people unawares – infecting many before they had time to have their annual vaccine. It was also characterised by having two peaks, caused by two different viruses which dominated at different times during the winter months. The southern hemisphere flu season is often seen as an early warning of what can be expected in Europe and the US.
Pregnant women, older people, and those with chronic conditions have at least one thing in common: they are at higher risk of complications if they catch a flu virus this winter. They are also more likely than average to come into contact with their community pharmacists as they collect medicines or seek advice.

That is why seven European countries have empowered pharmacies to deliver flu vaccination. Ireland, Portugal, France, Denmark, Switzerland, Norway and the United Kingdom all allow pharmacists to administer vaccines if they have completed a relevant training course, according to the PGEU which represents community pharmacies. It is already common practice in the US, Australia and elsewhere.
Ireland has perhaps the most experience in Europe, having begun pharmacy-based flu vaccination in 2011. The number of people vaccinated in pharmacies in Ireland has increased every year for eight years, now accounting for almost 15% of all flu vaccinations.
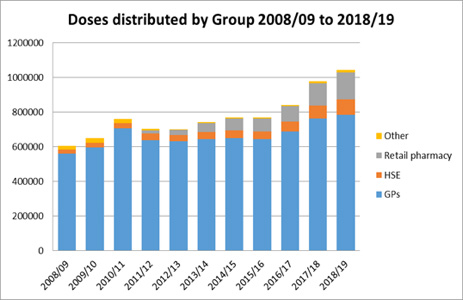
Table 1: GPs deliver most flu vaccinations in Ireland but the contribution of pharmacists is growing. Overall uptake has also risen.
However, the total number of people vaccinated has also increased, suggesting that pharmacists are reaching ‘new’ people rather than simply vaccinating those who would otherwise have been immunised by GPs or in hospitals.
‘Pharmacies offer greater convenience including expanded hours of operation, more flexible scheduling than other providers, and multiple locations near where people live,’ says Pamela Logan of the Irish Pharmacy Union.
‘Since pharmacists first started vaccinating, flu vaccine deliveries have increased overall by 48%. Deliveries [of flu vaccines] to GPs are up by almost 23%, demonstrating that when pharmacists vaccinate, public awareness increases and vaccination rates increase.’
 Research carried out by the Pharmaceutical Society of Ireland (PSI) has shown that patient satisfaction with the pharmacy flu vaccination service is high, with 99% of respondents rating their overall satisfaction as either 8, 9 or 10 out of 10.
Research carried out by the Pharmaceutical Society of Ireland (PSI) has shown that patient satisfaction with the pharmacy flu vaccination service is high, with 99% of respondents rating their overall satisfaction as either 8, 9 or 10 out of 10.
Ms Logan believes pharmacists can be powerful advocates for immunisation, particularly when engaging with people in risk groups. ‘Healthcare workers are the most trusted source for information about vaccines and every conversation with a patient or customer is an opportunity to promote vaccination,’ she says. ‘All of us in healthcare should take that opportunity to ensure that our patients and their families are protected from the risks of flu.’
Easing pressure on hospitals
By improving vaccination rates, pharmacies can help ease pressure on GP surgeries and hospital emergency departments which can become overcrowded in the event of serious influenza outbreaks. And, after a severe flu season in the southern hemisphere, Europe is braced for what could be a larger epidemic than last winter.
Several European pharmacy groups have taken inspiration from Ireland, Portugal, the UK and other early movers in the pharmacy sector.
‘An increasing number of pharmacy organisations in EU Member States have taken an interest in pharmacy vaccination following the success of the Irish pharmacy vaccination service,’ says Ms Logan. ‘A pharmacy vaccination pilot in France was so successful that the service has now been rolled out nationally. The IPU is willing to assist any pharmacy organisation in implementing a pharmacy vaccination service.’
Isabelle Guillaume of the French Chamber of Pharmacists says last winter’s pharmacy flu vaccination pilot led to 753,560 people being vaccinated in four regions of France. A new 2019 Social Insurance Budget Law, adopted in December 2018, added vaccination to the list of legal missions of pharmacists. It provides for national rollout of flu vaccination from 2019-2020.
Meanwhile, a pilot project in Portugal, designed to make it easier and cheaper for citizens to avail of pharmacy vaccination, increased vaccination rates by one third. The project allowed people to be vaccinated without prescription and without paying an administration charge.
While flu vaccination is the most commonly delivered vaccine in community pharmacies, others may be on the horizon. Ireland previously passed legislation expanding the rights of pharmacists to offer further immunisation services and, from this year, will pay pharmacists for providing pneumococcal vaccination to eligible patients.
Will pharmacy-based vaccination become the norm in all European countries? With almost all EU Member States falling short of their target to vaccinate 75% of older people against flu, it seems an option worth considering.




