One in 10 children globally has received no vaccines. For many, this has little to do with confidence in vaccines or complacency about the threat of infectious diseases. It’s about convenience – and access to basic healthcare.
A key barrier to accessing vaccination is the need to deliver vaccines to people in remote areas where infrastructure can be sorely lacking. Think of rural villages in Sudan or the mountainous regions of Afghanistan. Roads may be slow and treacherous; electricity supplies are often unreliable.
All of this matters because vaccines must be stored at a cool, stable temperature. Rapid transportation in refrigerated containers, and fridges to store them in upon arrival, are vital to preserving the ‘cold chain’.
In some parts of the world, health authorities and international agencies deliver vaccines by car, motorbike and even using drones. Researchers have been trying to find new ways to solve the problem, including by developing vaccines in powder form which may be easier to store and transport.
Eureka moment
Now, researchers at Bristol University, the French National Centre for Scientific Research (CNRS) and computer technology giant Oracle have hit upon a solution: using the latest in synthetic biology to produce thermostable vaccines.
A new kind of vaccine that needs no refrigeration勞!
Our scientists from @BrisBioDesign used synthetic biology & @Oracle cloud computing to yield results that could revolutionise vaccine development. #VaccinesWork #LoveBristolUnihttps://t.co/W0GOMg1fSB pic.twitter.com/PJDoVGPweg
— Bristol University (@BristolUni) September 26, 2019
Their discovery arose from a combination of knowledge, dedication and serendipity. While working on a new Chikungunya vaccine candidate, the team happened across a totally new way to engineer proteins. Their discovery could revolutionise the way vaccines are designed, produced and stored.
‘We were working with a protein that forms a multimeric particle resembling a virus but is completely safe, because it has no genetic material inside,’ said Pascal Fender, expert virologist at CNRS. ‘Completely by chance, we discovered that this particle was incredibly stable even after months, without refrigeration.’
The protein has a very flexible, exposed surface that can be easily engineered, added Imre Berger, Director of the Max Planck-Bristol Centre for Minimal Biology in Bristol. ‘We figured that we could insert small, harmless bits of Chikungunya to generate a virus-like mimic we could potentially use as a vaccine.’
The finding was published in a leading journal and will spark a flurry of research activity. ‘I think this is an example of a step-change,’ said Professor Adam Finn at the University of Bristol. ‘Up until now we have had to accept the materials that biology gives us. This represents a more deliberate attempt to actually engineer the bits and pieces that you need to make a vaccine work.’
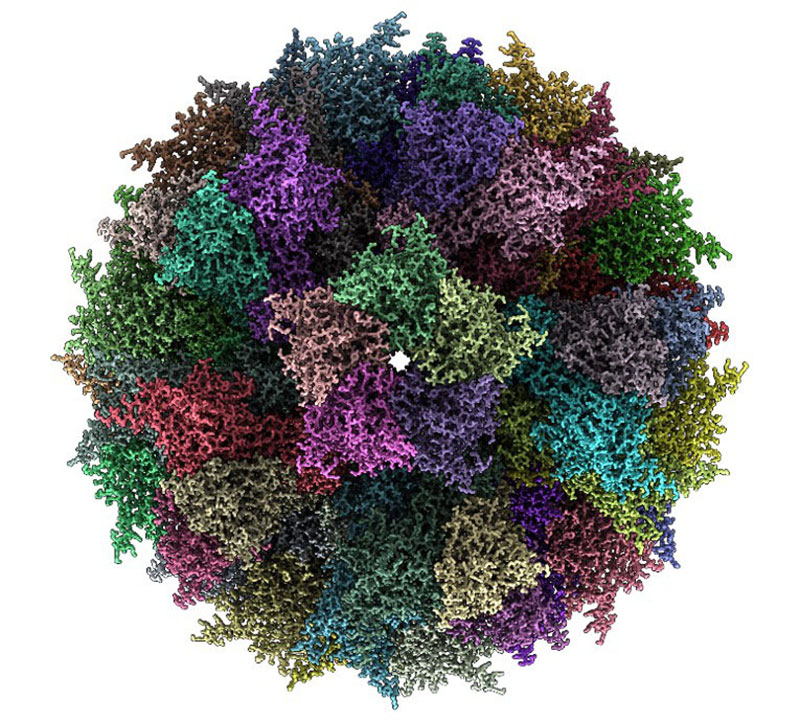
ADDomer: Synthetic multiepitope display scaffold for next generation vaccines. Image courtesy of University of Bristol
The particle the scientists designed has shown exceptionally promising results in animal studies, setting the stage for a future human vaccine to combat Chikungunya disease. It will be several years before any vaccine passes the clinical trials and regulatory tests required of any new vaccine but it would be a welcome new preventative tool, particularly in low-income countries.
Chikungunya, a virus transmitted by the bite of an infected mosquito, causes crippling headache, vomiting, swelling of limbs and can lead to death. Even if a fever ends abruptly, chronic symptoms such as intense joint pain, insomnia and extreme prostration remain.
Formerly confined to sub-Saharan Africa, Chikungunya has recently spread worldwide as its mosquito host leaves its natural habitat due to deforestation and climate change, with recent outbreaks in Europe and the US causing alarm.
The discovery of this new method could lead to the development of vaccines against other diseases, and perhaps even to new forms of existing vaccines.



